Fatty liver disease is exactly what the name suggests – a disease characterized by the build up of fat in the liver. There are two main types of fatty liver disease:
- Nonalcoholic fatty liver disease
- Alcoholic fatty liver disease (also called alcoholic steatohepatitis)
Both types of fatty liver disease are diagnosed when fat makes up at least 10% of the liver, but the cause of the fat build up is different for each type.
The cause of alcoholic fatty liver disease is obvious. The amount of alcohol it takes to cause fatty build up in the liver, however, is not so obvious. The Liver Foundation suggests consuming no more than 14 drinks a week for men and 7 drinks a week for women. Anything more than may cause fat to build up in the liver.
The treatment for alcoholic fatty liver disease is simple enough — stop drinking alcohol. Studies confirm that cessation of alcohol consumption can reverse alcoholic fatty liver disease.
However, the cause and treatment of nonalcoholic fatty liver disease are not as obvious. This is because many different factors (other than alcohol) can cause fat to build up in the liver.
The Truth About Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease affects 20-30% of adult populations in developed countries, but the mechanisms underlying its cause are incompletely understood. We can, however, take some clues from other common diseases to figure out why this happens.
In epidemiological studies including people with type 2 diabetes, 62 to 69% of them also had nonalcoholic fatty liver disease. Another study found that 50% of patients with dyslipidemia (abnormally elevated cholesterol levels) had nonalcoholic fatty liver disease.
Obesity, metabolic syndrome, and heart disease are also closely linked with nonalcoholic fatty liver disease. In fact, the most common cause of death for nonalcoholic fatty liver disease patients is heart disease.
This leaves us with five conditions that are commonly associated with nonalcoholic fatty liver disease: type 2 diabetes, obesity, heart disease, dyslipidemia, and metabolic syndrome.
What is even more intriguing is that obesity, type 2 diabetes, heart disease, dyslipidemia, and metabolic syndrome all are intimately linked as well. This is because they can all be caused by a combination of lifestyle, genetics, and gut health issues. Scientists believe that the same is true for nonalcoholic fatty liver disease as well.
What Causes Nonalcoholic Fatty Liver Disease?
The exact mechanisms that cause nonalcoholic fatty liver disease are not fully understood, but we do know for certain that lifestyle, genetics, and gut health issues play an important role.
1. Lifestyle — Eating Too Much and Exercising Too Little
Insulin resistance is a common side effect of eating too much and exercising too little, and it is one of the main reasons why fat builds up in the liver. Throughout the body, insulin resistance causes fatty acids to be released from fat cells and sugar to build up in the blood. The excess fatty acids and sugar (from the blood and the diet) enter the liver where they are converted into fat and stored.
As long as the liver, muscles, and adipose cells are resistant to insulin, sugar will continue to build up in the blood and fat will continue to build up in the liver. This vicious cycle of insulin resistance and fat accumulation in the liver is caused by eating too much and exercising too little.
Overfeeding on fat and sugar fills the cells up with energy to the point where they no longer respond to insulin. The liver receives the excess fat and sugar and has to store it has fat to save the body from the detrimental effects of having too much fat and sugar in the blood.
The quickest way to increase fat build up in the liver is by overfeeding on carbohydrates. Fructose, especially, will lead to the most fat accumulation in the liver. (Keep this in mind for when we go over the ideal fatty liver diet later.)
Having a sedentary lifestyle will also make your cells less sensitive to insulin. In fact, studies show that sitting for 2 hours after eating a meal can impair insulin sensitivity and increase blood sugar levels. Imagine what happens to you when the majority of your time is spent sitting and the majority of your meals consist of an overwhelming amount of carbohydrates and fat.
This is why many researchers agree that improving insulin sensitivity is a key strategy in the treatment of nonalcoholic fatty liver disease. However, there is a small subset of people who can get nonalcoholic fatty liver disease without showing any signs of insulin resistance.
2. Genetics — Gene Variants, Gender, and Ethnicity
Like many common diseases, nonalcoholic fatty liver disease is polygenic. This means that the interaction of many different gene variants can make someone more susceptible to having a fatty liver.
One genetic variant, in particular, that is called PNPLA3 I148M is associated with the development of nonalcoholic fatty liver disease without the presence of obesity, diabetes, dyslipidemia, or insulin resistance.
However, just because you have the gene does not mean you will have the disease. For example, the PNPLA3 I148M gene variant will only lead to disease progression in combination with alcohol abuse, unhealthy diet, high levels of fructose consumption, inactivity, or viral infection.
The fact that nonalcoholic fatty liver disease has a polygenic basis also provides us with a possible explanation for why nonalcoholic liver disease tends to be found in clusters of family members. This is why it is of the utmost importance to develop healthy lifestyle habits if your parents and grandparents struggled with nonalcoholic fatty liver disease.
Other genetic factors like your gender and ethnicity impact your likelihood of developing fatty liver disease as well. Although older studies found that women were at greater risk for fatty liver disease, current studies found that it is more prevalent in men.
Scientists postulate that this is due to the difference in hormones and fat distribution between men and women. Men tend to store more fat near their organs, which is a type of fat that is more inflammatory. This increases the risk of many common diseases like heart disease, diabetes, and nonalcoholic fatty liver disease.Women, on the other hand, tend to accumulate fat in their hips and thighs, which is much less inflammatory.
When it comes to ethnicity, studies have found that African Americans have the lowest risk of nonalcoholic fatty liver disease, despite having a higher risk of type 2 diabetes. Once again, this is thought to be because of the fact that they tend to store fat away from their organs.
Conversely, Asians and Hispanics seem to have the highest risk of nonalcoholic fatty liver disease. Researchers think that this is because they tend to store fat near their organs more than other ethnicities.
Another important thing to mention is the effect that other genes have on the development of fatty liver disease. I am not talking about your genes. It’s time to move on to the genes in your microbiome.
3. Gut Health Issues — Your Microbiome and Nonalcoholic Fatty Liver Disease
Your microbiome is made of 100 trillion bacteria that line your gut. The types of bacteria that flourish or perish have a substantial impact on your health, especially the health of your liver.
Studies done on the microbiome of obese patients found that they had a reduced abundance of a type of bacteria called Bacteroidetes and an increased abundance of another bacteria called Firmicutes. This ratio of Bacteroidetes to Firmicutes led to an increase in lipopolysaccharide absorption.
What are lipopolysaccharides? They are a component of the cellular membrane of gram-negative bacteria like Bacteroidetes. However, they aren’t as harmless as they sound.
Lipopolysaccharides are endotoxins that trigger a potent inflammatory response in the body. This response contributes directly to insulin resistance in the liver and obesity.
Although everyone’s microbiome is unique, there seems to be a clear answer to where this obesity inducing microbiome comes from. The answer is — an obesity producing diet. More specifically, a high-sugar, high-fat diet.
This kind of diet reduces the diversity of the microbiome, favoring an increase in the Firmicutes-to-Bacteroidetes ratio in the gut. The result will be an obesity-causing microbiota profile that favors the development of obesity and fatty liver disease.
However, this isn’t the worst of it. The increase in lipopolysaccharides absorption caused by a poor diet and an obesity-causing microbiome can disrupt the liver so much that nonalcoholic fatty liver disease progresses to nonalcoholic steatohepatitis.
Nonalcoholic Steatohepatitis — When The Bad Gets Worse
Having some extra fat in the liver isn’t going to cause any problems for 70-80% of people with fatty liver disease. However, when the cause of that fat build up gets worse, it can lead to nonalcoholic steatohepatitis.
This form of fatty liver disease affects 20-30% of patients with nonalcoholic fatty liver disease, and it occurs when the build up of fat in the liver leads to inflammation that can result in liver cell damage.
Not everyone with a fatty liver will eventually develop nonalcoholic steatohepatitis. Many factors determine whether fatty liver will lead to liver damage, including:
- Oxidative stress
- Mitochondrial abnormalities
- Hormonal disturbance
- Lipotoxicity
To simplify these complex terms, fatty liver disease goes from bad to worse when the lifestyle and microbiome that caused the build up of fat in the liver continue. We know for certain (thanks to many studies) that excessive calorie consumption, excess fructose consumption, and a sedentary lifestyle cause fat to build up in the liver and elsewhere in the body.
The fat cells eventually become overloaded and begin to secrete inflammatory cytokines. These inflammatory cytokines increase inflammation levels and cause reactive oxygen species to accumulate (oxidative stress). As poor lifestyle choices continue, so much fat builds up in the liver that it leads to lipotoxicity (accumulation of fat in non-fat cells). The combination of lipotoxicity and oxidative stress can cause hormonal disturbances and liver damage.
Meanwhile, in the gut, the fatty liver disease promoting lifestyle changes the microbiome. This increases inflammation, oxidative stress, and lipopolysaccharide absorption, which causes more liver damage.
Having certain genetic mutations can also increase the risk of developing nonalcoholic steatohepatitis. For example, carriers of the PNPLA3 I148M gene variant (that we mentioned earlier) and the TM6SF2 E167K variant seem to be at a greater risk for nonalcoholic steatohepatitis.
However, even if you have specific gene variants that increase your chances of fatty liver disease and liver damage, you are not doomed to get nonalcoholic steatohepatitis. This is because, like type 2 diabetes, obesity, and heart disease, fatty liver disease is reversible. Plus, there is even better news — type 2 diabetes, obesity, heart disease, and fatty liver disease can all be reversed with the same lifestyle changes.
How To Reverse Nonalcoholic Fatty Liver Disease
The key to disrupting the vicious cycle of fatty liver disease before it damages the liver is exercise and diet.
That’s right — Treating obesity of the liver is similar to treating obesity of the body. In fact, many scientific papers agree that the treatment of nonalcoholic fatty liver disease should be focused on controlling diabetes, obesity, insulin resistance, and hyperlipidemia. We should only focus on treating the liver in those with nonalcoholic steatohepatitis.
This means that the best way to reverse nonalcoholic fatty liver disease and prevent liver damage is with a diet that has been proven to control diabetes, obesity, insulin resistance, and hyperlipidemia.
Luckily, this diet already exists and has been found to more effective than caloric restriction and low-fat diets. This diet is called the ketogenic diet. A diet that focuses on restricting carbohydrates, removing one of the main drivers of fatty liver disease from the diet.
However, we cannot call the ketogenic diet the ideal diet for fatty liver disease yet. This is only a theory that is based on evidence for how the ketogenic diet helps people with issues related to nonalcoholic fatty liver disease. To see what works best for the disease itself, we must dig through the research.
What Is The Best Fatty Liver Reducing Diet and Lifestyle?
In a review of studies on nonalcoholic fatty liver disease treatments, the researchers found that weight loss leads to a substantial improvement in the disease. Weight loss of 3-5 % improves fatty liver disease, but to reduce inflammation and liver damage, a weight loss of 10% may be needed. To accomplish this, researchers used the most well-known way to promote weight loss: caloric restriction and exercise.
Let’s start with exercise. Physical activity alone improves insulin sensitivity and reduces fat in the liver.
In fact, one study kept the body weight of their subjects constant while they implemented an exercise training program. They found that it leads to a distinct decrease in liver fat.
In studies that combine caloric restriction with exercise, the results are even more promising. For example, one study took twenty-five obese patients with fatty liver and put fifteen of them on a calorie restricted diet and exercise program for 3 months.
The calorie restricted diet was based on a daily calorie intake of the patient’s ideal weight in kilograms multiplied by 25 calories, and the exercise program is described as “walking or jogging”.
The researchers found that the treatment group’s “weight, blood biochemical data such as aminotransferase, albumin, cholinesterase, total cholesterol and fasting blood glucose values, and steatosis (fatty liver) were significantly decreased after the trial. In the control group, there were no significant differences in the clinical and histological findings before and after the trial.”
It’s that simple. Eat less and move more, and you can reverse fatty liver disease. Many review articles on the treatments for nonalcoholic fatty liver disease also agree on this simple principle, but they don’t agree upon what kind of exercise to do.
Many studies have been done on different types of exercise and their effects on fatty liver disease, but there is not enough data to come to a clear conclusion about what is best. However, we do know what is better — doing the exercise that you will actually do.
The jury is still out on the best diet for nonalcoholic fatty liver disease as well. We know for certain that restricting your calories helps, but another diet may provide even better results, making it worthy of the name “fatty liver diet”.
The Ketogenic Diet May Be The Best Fatty Liver Diet
We mentioned before that weight loss is essential when reversing nonalcoholic fatty liver disease, and an even greater reduction in weight loss is helpful for patients with nonalcoholic steatohepatitis. The best way to achieve this weight loss, however, is not with caloric restriction.
In fact, many studies conclude that caloric restriction is inferior to a low-carbohydrate, ketogenic diet when it comes to weight loss. For example, one study split 132 people into two groups: a low-carbohydrate diet (30 grams or less of carbohydrates a day) group and a calorie-restricted, low-fat diet group.
After six months of this dietary intervention, the researchers concluded that “severely obese subjects with a high prevalence of diabetes and the metabolic syndrome lost more weight in a six-month period on a carbohydrate-restricted diet than on a fat- and calorie-restricted diet.”
The ketogenic diet has also been proven in multiple studies to be more effective than a calorie-restricted diet at reversing type 2 diabetes, obesity, heart disease, and hyperlipidemia. This must mean that it is effective for nonalcoholic fatty liver disease as well, right?
A recent pilot study put five patients on the ketogenic diet ( less than 20 grams per day of carbohydrate). At the end of six months, the average weight loss was 28 pounds, but this wasn’t the most surprising finding. Each patient underwent a liver biopsy, and four of the five patients showed a reduction in liver fat, inflammation, and fibrosis. This provides preliminary evidence that the ketogenic diet can reverse fatty liver disease and nonalcoholic steatohepatitis.
However, this is a small pilot study (and the patients took supplements as well). To get a clear answer, we must find more studies on the ketogenic diet and fatty liver disease.
In a 2016 meta-analysis and systematic review on the effects of low carbohydrate diets on liver function tests in nonalcoholic fatty liver disease patients, the researchers’ conclusions were not as promising.
They found that the low carbohydrate diet decreased fat in the liver significantly, but the liver function tests did not improve. The measurements they looked at to determine liver function were the liver enzymes (AST, ALT, and GGT) that are usually elevated in patients with nonalcoholic fatty liver disease. As a result of the low carbohydrate diet, these levels decreased, but not enough to be statistically significant.
When we look more closely at the studies in the meta-analysis, they either found no effect on liver enzyme levels or a significant effect. In other words, the liver function of some people stayed the same on the low-carbohydrate diet while others improved significantly. Why the difference?
Two factors that we talked about earlier could be at the root of the differences between studies. These factors are genetics and gut health.
Some people were born with a set of genetic variants that make it harder for them to adapt to the low carbohydrate diet, which may lead to a minimal improvement of liver function. It is possible, however, that these people could get better results if they stay with the diet longer.
Gut health is another important variable to consider. When many people first try a high-fat, low-carb diet, they may focus on all of the fatty meat and cheese they can eat and forget about eating vegetables. Excess fat consumption with very little fiber can cause the gut microbiome to change tremendously. This leads to more lipopolysaccharides being absorbed and more inflammation in the body and the liver.
To optimize your diet to reverse disease, especially fatty liver disease, it is imperative to have low-carbohydrate vegetables with every meal. The combination of vegetables and carbohydrate restriction is what makes an ideal fatty liver diet.
The Best Fatty Liver Diet
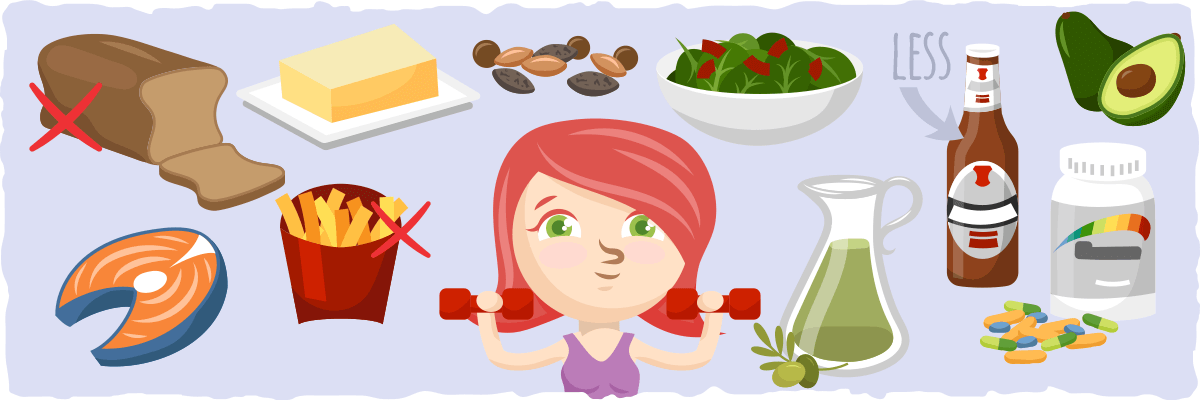
The ketogenic diet is a good diet for reversing fatty liver disease, but you can make it the best fatty liver diet by following these guidelines:
1. Restrict Carbohydrates to 5% of Your Daily Calories
By doing this, you will greatly reduce the likelihood that your liver with convert excess energy into fat. You will also reduce insulin, blood sugar, and inflammation levels that would otherwise cause liver issues.
For more on how to restrict your carbohydrates and follow the ketogenic diet properly, look through our comprehensive beginner’s guide to the ketogenic diet.
2. Eat High-Fiber Foods With Every Meal
The healthiest way to get more fiber is by consuming low-carbohydrate vegetables. They will improve gut health, reduce the absorption of harmful lipopolysaccharides, and improve the health of the cells throughout your body.
Here are some examples of high-fiber ketogenic salads that you can try :
Or you can pair your favorite meal with a low-carbohydrate vegetable side dish like one of these:
- Easy Creamed Spinach
- Mashed Cauliflower with Parmesan
- Au Gratin Brussels Sprouts
- Lemon Roasted Spicy Broccoli
For more on what vegetables to eat on the ketogenic diet, check out our vegetable guide for ketogenic dieters.
3. Eat Liver Healing Foods
You can also add these five scientifically-proven liver healing foods to your diet to help reverse fatty liver disease:
- Oily Fish
Two or more servings of oily fish per week can have a beneficial effect on blood lipids and may reduce liver fat. Wild-caught salmon is one of the healthiest oily fish you can have.
- Regular Filtered Unsweetened Coffee
Coffee is associated with reduced fibrosis severity in nonalcoholic fatty liver disease.
- Nuts
A handful of nuts per day improves liver function tests. Walnuts, in particular, have been found to be one of the healthiest nuts for your liver.
- Avocado
Avocado consumption is associated with weight loss and improved liver tests. This is mainly because avocados have a substantial amount of monounsaturated fat, fiber, and antioxidants.
- Olive Oil
This popular oil improves liver function tests and helps with weight loss because it is loaded with antioxidants and oleic acid.
4. Use Liver Healing Supplements
When you search the internet for liver supplements, you are inundated by supplements that seem promising, yet have no shred of evidence that backs of their claims. To save you some time and experimentation, here are three supplements that have been found to improve liver health:
- Spirulina
Spirulina is a natural algae powder that is incredibly high in protein and a good source of antioxidants, B-vitamins, and other nutrients. A dose of 4.5 grams (about a teaspoon) per day of spirulina has been shown to help reverse fatty liver disease.
- Betaine
Betaine is a compound that is naturally found in beets and spinach. It is essential for the normal function of the blood, bones, eyes, heart, nerves, and the brain, and it reduces build up of fat in the liver.
The best way to supplement with betaine is by eating raw beets (not keto-friendly) or taking a TMG supplement. TMG stands for Trimethylglycine, and it is the form of betaine that is found in beets.
- Milk Thistle
Milk thistle contains a compound called silybin. Silybin can reduce fat build up in the liver, and it may even reverse liver damage.
- Probiotics
In a meta-analysis on the effects of probiotics on nonalcoholic fatty liver disease, researchers found that probiotic therapy can help improve liver function and reduce inflammation. But, not just any probiotic will do.
Bifidobacterium longum seems to be the most effective probiotic strain at reducing liver fat, inflammation, and endotoxin levels. Lactobacillus GG, Lactobacillus bulgaricus, and Streptococcus thermophilus were helpful in reversing nonalcholic fatty liver disease as well.
5. Limit Alcohol Consumption
Although no alcohol consumption is best for reversing nonalcoholic fatty liver disease, some alcohol consumption may be beneficial as well. In fact, one nonalcoholic fatty liver disease treatment review found that limiting alcohol consumption to less than one drink per day may actually have a beneficial effect on liver health.
6. Exercise Everyday
The kind of exercise that is best for reversing fatty liver disease is not yet known, but almost any type of exercise will help. It is probably best to go for brisk walks throughout the day and do resistance training at least 3 times a week.
But don’t get caught up in finding the perfect workout plan. Any exercise is better than no exercise for all aspects of health. Start by doing what you enjoy doing.
Sample Fatty Liver Diet Plan Menu
To give you a better idea of what this diet would look like, here is a menu of low carb recipes featuring liver-healthy foods:
For Breakfast:
- Ketoproof Coffee — Blend healthy keto fats into your coffee for a quick breakfast that’ll keep you energized through lunch. (Not a fan of coffee? Try adding fat to your tea)
- Keto Granola Cereal — The perfect cereal if you are looking to cut out the sugar and eat more nuts and fiber.
- Keto Meal Replacement Shake — A delicious way to sneak in a quick keto meal with avocado.
- Salmon Benny Breakfast Bombs — This combination of salmon, eggs, and bacon with hollandaise sauce is an incredible way to start the day.
For Lunch:
- Keto Smoked Salmon Filled Avocados — This quick keto lunch gives you a hearty portion of avocado and salmon, which both help support liver health.
- Keto Chicken, Bacon, and Avocado Salad — A delicious way to fit some extra low-carb veggies and avocado into your fatty liver diet plan.
- Grilled Tuna Salad with Garlic Dressing — A unique and satisfying keto salad recipe featuring walnuts, tuna, garlic, asparagus, and greens.
- Spinach, Herb & Feta Wrap — Try this fresh, savory keto wrap if you want a lunch packed with flavor. Don’t forget to add a drizzle of EVOO for an extra boost of liver-healthy fats and antioxidants.
For Dinner:
- Spicy Cauliflower Rice & Salmon Medley — A quick and easy low-carb salmon fried rice with plenty of spice.
- Nacho Steak Skillet — Mexican-inspired keto skillet with plenty of low-carb vegetables and avocado.
- Zucchini Ribbons & Avocado Walnut Pesto — A vegetarian keto pasta dish that shows you how to use liver healing foods to make veggies taste delicious.
- Low Carb Walnut Crusted Salmon — A simple salmon dish featuring walnuts and olive oil. For a complete meal, serve it with one of the low-carb vegetable side dishes listed in the previous section.
For Dessert:
- Chocolate Chunk Avocado Ice Cream — 100% sugar-free keto-friendly ice cream that gets its silky smooth texture from avocado.
- Luscious Caramel Pecan Pie — Packed with low-carb nuts and healthy fats, this pecan pie is perfect for satisfying your sweet tooth without slowing your progress.
- Keto Avocado Brownie — One of my favorite ways to add some extra liver-healthy avocado into my diet.
Quickstart 3-day Fatty Liver Diet Plan
Here is a quick and simple example of what each meal would look like while implementing the information found throughout this article:
Day 1: For the Breakfast Lovers
Breakfast: 1-2 servings of Salmon Benny Breakfast Bombs
Lunch: 1-2 servings of Keto Chicken, Bacon, and Avocado Salad
Dinner: 1 serving of Low Carb Walnut Crusted Salmon with a side of 1-2 servings of Lemon Roasted Spicy Broccoli
Dessert (optional): 1 Keto Avocado Brownie
Day 2: All Vegetarian-friendly Keto Meals
Breakfast: 1 serving of the Keto Meal Replacement Shake
Lunch: 1 Spinach, Herb & Feta Wrap
Dinner: 1-2 servings of Zucchini Ribbons & Avocado Walnut Pesto
Dessert (optional): 1 serving of Luscious Caramel Pecan Pie
Day 3: A Taste of Intermittent Fasting
Breakfast: 1 serving of Ketoproof Coffee
Lunch: 1 serving of Grilled Tuna Salad with Garlic Dressing
Dinner: 1-2 servings of Nacho Steak Skillet
Dessert (optional): 1 serving of Chocolate Chunk Avocado Ice Cream
Please note: This sample fatty liver diet plan is not one-size-fits-all. We designed this to show you what three days of keto eating can look like.
To ensure that you reach your health and weight loss goals, you must adjust your meals and servings based on your keto macro needs (our keto calculator can help you figure this out).
The easiest way to tailor the keto diet to your needs is by using our keto diet plan app. Simply enter your info, goals, and preferences, and it will provide you with a personalized long-term meal plan.
Is it Possible to Reverse Fatty Liver Disease Completely? A Keto Success Story Testimonial
By using what you’ve learned throughout this article, evidence suggests that you can lose belly and liver fat at the same time.
However, one crucial question still remains unanswered: Is this simple diet change enough to completely reverse fatty liver disease?
Christine is living proof that this is possible. Before trying keto, she was overweight with NAFLD, obstructive sleep apnea, and on the verge of type 2 diabetes.
No diet plan provided lasting results, and even a “Diabetes Prevention Program” failed to help her. Once she found out about keto, however, everything changed.
After just over a year of keto eating, her results are astonishing:
- No more obstructive sleep apnea
- No more non-alcoholic fatty liver disease (confirmed by ultrasound)
- Achieved her goal weight (after 95 lbs of weight loss!)
- Feels better than she did at 30
Believe it or not, this is only a brief snippet of what she shared with us in her success story — and all she did was switch to the keto diet.
What About Using Drugs for Fatty Liver Disease?
For a typical nonalcoholic fatty liver disease patient, pharmaceutical drugs are not usually recommended. However, when the disease progresses to liver-damaging nonalcoholic steatohepatitis drug therapy may be necessary.
Metformin, a common diabetes drug, has been tested many times for fatty liver disease, but it has no significant effect on liver cells.
A drug called thiazolidinedione, however, has been shown to be effective for improving diabetes, liver function, and fibrosis of the liver. The only problem with the drug is that patients relapse when they aren’t on it.
In a study that tested thiazolidinedione in the treatment of nonalcoholic steatohepatitis, researchers found that diet and exercise were essential in maintaining the results achieved by drug therapy.
When patients in the study followed up after 37 months, the patients who had sustained exercise programs and reduced their body mass index, also had normal liver enzyme levels, fibrosis improvement, and were free from diabetes. On the other hand, patients who made no lifestyle changes had gotten worse after discontinuing the drug.
Putting It All Together
Nonalcoholic fatty liver disease affects 20–30% of adult populations in developed countries. The build-up of fat in the liver is harmless at first, but it can lead to nonalcoholic steatohepatitis (inflammation and liver damage).
Fatty liver disease is so intimately associated with type 2 diabetes, obesity, hyperlipidemia, metabolic syndrome, and heart disease that it is believed to be caused by the same factors. These factors are an unhealthy lifestyle, genetics, and gut health issues (an obesity and inflammation causing microbiome).
Although genetics can’t be changed, almost everyone can prevent and reverse fatty liver disease with the right diet and exercise program. Research suggests that the right diet is a low carbohydrate and high fiber diet. The perfect example of this is the ketogenic diet. This diet maintains a healthy gut microbiome and limits fructose and carbohydrate (the two dietary components that cause fat to build up in the liver), which makes it the ideal fatty liver diet.
When it comes to exercise, many different forms of activity from walking to lifting weights can help reverse fatty liver disease. Do some form of activity every day for best results.
The combination of the ketogenic diet and exercise makes a great treatment for fatty liver disease, but they aren’t the only important things that can help reverse the disease. Limiting alcohol intake, eating low-carbohydrate vegetables like spinach and kale, taking liver healing supplements like spirulina and milk thistle, and including liver healing foods in your diet are essential in reversing fatty liver disease as well.
When you put it all together, here is an overly simplified version of the best fatty liver diet and lifestyle plan:
- Restrict carbohydrates
- Eat low-carbohydrate vegetables with every meal
- Exercise every day
- Take scientifically-proven liver healing supplements like spirulina, betaine, and milk thistle
- Include liver healing foods in your diet like avocado, nuts, oily fish, olive oil, and unsweetened coffee
- Limit alcohol intake
Sources:
- The diagnosis and management of non-alcoholic fatty liver disease: Practice Guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association — Wiley Online Library
- Treatment of non-alcoholic fatty liver disease — BMJ Journals
- Non-alcoholic fatty liver disease: an overview of prevalence, diagnosis, pathogenesis and treatment considerations — Clincial Science
- The Natural History of Nonalcoholic Fatty Liver Disease: A Population-Based Cohort Study — Science Direct
- New-found link between microbiota and obesity — NCBI
- Association between composition of the human gastrointestinal microbiome and development of fatty liver with choline deficiency. — NCBI
- Eubiosis and dysbiosis: the two sides of the microbiota. — NCBI
- The Pathogenesis of Nonalcoholic Fatty Liver Disease: Interplay between Diet, Gut Microbiota, and Genetic Background — Hindawi
- A meta-analysis of randomized trials for the treatment of nonalcoholic fatty liver disease. — NCBI
- Effects of exercise training on intrahepatic lipid content in humans — Springer Link
- The effects of low carbohydrate diets on liver function tests in nonalcoholic fatty liver disease: A systematic review and meta-analysis of clinical trials — NCBI
- The Effect of a Low-Carbohydrate, Ketogenic Diet on Nonalcoholic Fatty Liver Disease: A Pilot Study — Springer Link
- Therapeutic effects of restricted diet and exercise in obese patients with fatty liver — Science Direct
- A Low-Carbohydrate as Compared with a Low-Fat Diet in Severe Obesity — The New England Journal of Medicine
- Effect of Vitamin E or Metformin for Treatment of Nonalcoholic Fatty Liver Disease in Children and Adolescents: The TONIC Randomized Controlled Trial — The JAMA Network
- A Randomized Controlled Trial of Metformin versus Vitamin E or Prescriptive Diet in Nonalcoholic Fatty Liver Disease — ProQuest
- Insoluble Dietary Fiber from Pear Pomace Can Prevent High-Fat Diet-Induced Obesity in Rats Mainly by Improving the Structure of the Gut Microbiota — JMB
- Hepatoprotective effects of Spirulina maxima in patients with non-alcoholic fatty liver disease: a case series — BioMed Central
- Spirulina improves non-alcoholic steatohepatitis, visceral fat macrophage aggregation, and serum leptin in a mouse model of metabolic syndrome — Science Direct
- Spirulina — Examine
- Sitting for just a couple hours has measurable (and negative) health impact — PLOS
- Oily fish, coffee and walnuts: Dietary treatment for nonalcoholic fatty liver disease — NCBI
- Avocados Contain Potent Liver Protectants — Science Daily
- Non alcoholic fatty liver disease and metabolic syndrome — NCBI
- Gender and racial differences in nonalcoholic fatty liver disease — NCBI
- Recent trends in the epidemiology of alcoholic liver disease — Wiley Online Library
- Metabolic Endotoxemia Initiates Obesity and Insulin Resistance — Diabetes Journals
- The Epidemiology of Nonalcoholic Fatty Liver Disease: A Global Perspective — Medscape
- Treatment of Nonalcoholic Fatty Liver Disease: Where do we Stand? An Overview — NCBI
- Physical activity as a treatment of non-alcoholic fatty liver disease: A systematic review — NCBI
- Long-term effects of a ketogenic diet in obese patients — NCBI
- Profile of liver enzymes in non-alcoholic fatty liver disease in patients with impaired glucose tolerance and newly detected untreated type 2 diabetes — NCBI
- Prebiotic fiber modulation of the gut microbiota improves risk factors for obesity and the metabolic syndrome — NCBI
- Milk Thistle — Examine
- Thiazolidinediones for the treatment in NASH: sustained benefit after drug discontinuation? — NCBI
- Effects of probiotics on nonalcoholic fatty liver disease: A meta-analysis — NCBI