For thousands of years, something has been sneaking up on children and robbing them of their ability to control their blood sugar levels. The culprit is an autoimmune condition called Type 1 Diabetes, and its incidence has been increasing in both the United States and in other western countries.
But there is no need to worry. This sneaky disease has left us with enough clues to diagnose it, manage it, and potentially reverse it. This can be done by type one diabetics following the keto diet.
How to Know If It Is Type 1 Diabetes
Type 1 diabetes is most commonly diagnosed in children between the ages of 10 and 14, although many children can present with symptoms at ages as young as two years old. The incidence is approximately 1.5 times higher in American non-Hispanic white people compared with African American or Hispanic individuals.
Risk Factors for Type 1 Diabetes
The three most well-researched risk factors for type 1 diabetes include:
- Family history. Anyone with a parent or sibling with type 1 diabetes has a slightly increased risk of developing the condition.
- Genetics. Specific genes can increase the risk of developing type 1 diabetes.
- Age. Although type 1 diabetes can appear at any age, it is diagnosed in two prominent peaks. The first peak occurs in children between 4 and 7 years old, and the second is in children between 10 and 14 years old.
However, these aren’t the only three risk factors. Recent research has found that type 1 diabetics tend to have a different balance of bacteria in their microbiome then non-susceptible individuals. Vitamin D deficiency, gut health issues, and dairy intolerance are also linked to a greater risk of type 1 diabetes as well.
Having all of these risk factors, however, does not mean that you will have type 1 diabetes. Its symptoms will provide us with a clearer picture.
Symptoms of Type 1 Diabetes
Type 1 diabetes signs and symptoms can appear relatively suddenly and may include:
- Increased thirst
- Frequent urination
- Bed-wetting in children who previously didn’t wet
- Extreme hunger
- Unintended weight loss
- Irritability and other mood changes
- Fatigue and weakness
- Blurred vision
If you see any of the above symptoms in you or your child, then consult your doctor right away. If not, symptoms may progress to diabetic ketoacidosis — the most common cause of death in children who have type 1 diabetes.
How to Confirm If It’s Type 1 Diabetes
At your doctor’s appointment, they will run some blood tests to get more clues as to what is going on.
These blood tests may include:
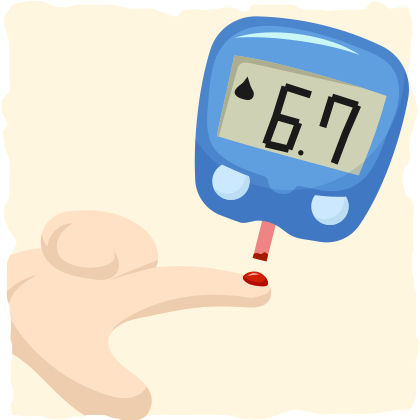
Glycated Hemoglobin (A1C) Test
This blood test indicates your average blood sugar level for the past two to three months. It measures the percentage of blood sugar attached to hemoglobin (the oxygen-carrying protein in red blood cells).
The higher your blood sugar levels, the more glycated hemoglobin you will accumulate. An A1C level of 6.5 percent or higher on two separate tests indicates diabetes.
Random Blood Sugar Test
Regardless of when you last ate, a random blood sugar level of 200 mg/dL (11.1 mmol/L) or higher suggests diabetes. This blood sugar level is especially suggestive of diabetes when coupled with any of the signs and symptoms of the condition, such as frequent urination and extreme thirst.
Fasting Blood Sugar Test
A blood sample taken after an overnight fast is a fasting blood sugar test. A fasting blood sugar level less than 100 mg/dL (5.6 mmol/L) is normal. A fasting blood sugar level from 100 to 125 mg/dL (5.6 to 6.9 mmol/L) is a pre-diabetic level. If it’s 126 mg/dL (7 mmol/L) or higher on two separate tests, then you have diabetes.
Autoantibody Testing
If you’re diagnosed with diabetes, your doctor may also run blood tests to check for autoantibodies that are common in type 1 diabetes. These tests help your doctor distinguish between type 1 and type 2 diabetes when the diagnosis is uncertain.
The Difference Between Type 2 and Type 1 Diabetes
Let’s clear up any questions you may have regarding type 1 and type 2 diabetes.
The type of diabetes we are focusing on for this article is type 1 diabetes. It accounts for about 5–10% of all cases of diabetes. Being an autoimmune disease, it turns the body’s immune system — which normally fights harmful bacteria and viruses — against the insulin-producing cells in the pancreas. Eventually, the immune system destroys the pancreas’s ability to produce insulin. The result is blood sugar levels that are out of control and wreak havoc on the body.
Type 2 diabetes, on the other hand, is a result of insulin resistance rather than insulin deficiency. Insulin resistance occurs when the cells no longer respond to insulin signaling. The pancreas responds by secreting more insulin, which increases insulin resistance in the cells. This vicious cycle creates chronically high blood sugar levels.
Type 2 diabetes is commonly caused by overfeeding on calories and carbohydrates (the macronutrient that stimulates the most insulin secretion) and inactivity, not by an autoimmune issue. However, both type 1 and type 2 diabetes have many similarities including their symptoms, long-term complications, and the diet that helps best with their treatment.
The Long-Term Complications of Diabetes
When left unmanaged, both type 1 and type 2 diabetes can affect major organs in your body, including heart, blood vessels, nerves, eyes, and kidneys. Eventually, diabetes complications may be disabling or even life-threatening.
The most common long-term complications of diabetes are:
- Cardiovascular disease
- Nerve damage (neuropathy)
- Kidney damage (nephropathy)
- Eye damage
- Foot damage
- Skin and mouth conditions
- Pregnancy complications
Although both type 1 and type 2 diabetes can be catastrophic, these long-term complications can easily be avoided. Substantial research evidence suggests that diabetic complications are decreased as a result of improved glycemic control.
In other words, if you control your blood sugar levels, they won’t control you.
How to Treat Type 1 Diabetes
When you improve your blood sugar levels (indicated by lower A1C and better blood sugar numbers), you will improve your health and be able to live a normal life with type 1 diabetes.
To improve blood sugar control, people with type 1 diabetes must:
- Take insulin and follow the treatment plan prescribed by the doctor
- Track carbohydrate, fat and protein intake
- Frequently monitor blood sugar with a blood sugar monitor
- Eat healthy foods
- Exercise regularly
- Maintain a healthy weight
This is what many doctors and researchers suggest, but “eat healthy foods” and “track carbohydrate, fat, and protein intake” are vague suggestions. Is there a specific diet plan that people with type 1 diabetes can follow?
The Type 1 Diabetes Diet
A 2008 article in the Pediatrics in Review contains all the recommendations for working with children with type 1 diabetes, including the ideal diet. What do they suggest?
The recommended diet usually contains 50% to 55% carbohydrate calories, 20% protein, and approximately 30% fat. Most carbohydrate calories should be complex carbohydrates, and the fat portion should emphasize low amounts of cholesterol and saturated fats.
However, studies on how this kind of diet affects patients with type 1 diabetes are nonexistent. Interestingly, the research suggests that there may be a better diet. In fact, it is the same diet that has been found to help reverse type 2 diabetes — the ketogenic diet.
The Evidence Points to The Ketogenic Diet for Type 1 Diabetes
The first line of evidence for an ideal type 1 diabetes diet is a pair of case studies: one with a young girl and another with an adolescent male.
The young girl in the first case study had epilepsy and type 1 diabetes, which is more prevalent in children with epilepsy. Researchers sought after an effective diet for this complicated case, so they put the girl on a classic ketogenic diet (about 5% daily calories from carbs and 75% from fat) for 15 months.
The results were promising. Since the start of the ketogenic diet, no clinically overt seizures were reported. The girl was even being much more active and reaching significant developmental achievements that she wasn’t reaching before the ketogenic diet.
The researchers also tracked the girl’s A1C levels and glycemic control, the two most important measures for type 1 diabetics. Both of them improved significantly without any adverse side effects. These results indicate that the ketogenic diet may help manage type 1 diabetes and epilepsy simultaneously.
The results of the other case study were even more incredible. In the study, a 19-year-old male with newly diagnosed type 1 diabetes was put on a special type of ketogenic diet for 6.5 months. During this period, he was able to discontinue insulin use and restore some of the insulin production in his pancreas.
The researchers went on to conclude that:
…an intervention with the paleolithic ketogenic diet in an early stage of the disease with residual insulin secretion may halt or reverse type 1 diabetes mellitus. Follow-up at sixth month in the case of our patient is relatively short and the positive results may appear as a honeymoon effect.
The honeymoon effect is the period of time when the pancreas is still producing enough insulin to aid blood glucose control. Because of the honeymoon effect, it is much more likely that the paleolithic ketogenic diet didn’t halt or reverse type 1 diabetes. However, the possibility that this diet is responsible for this patient’s incredible recovery still remains.
To get a more definitive understanding of these results, I reached out to the authors of the case study for an update on their patient’s condition. One of the researchers responded promptly with this:
No, it was not a honeymoon period. But he decided to stop the diet and therefore had to go back to insulin. Another patient with a much longer follow-up: Case Study
Although this indicates that type 1 diabetes was not reversed (in both cases), these results are still impressive — and the paleolithic ketogenic diet is the primary reason why.
But what exactly do the researchers mean by a “paleolithic ketogenic diet”?
Here’s how they described it:
His diet consisted of meat, organ meat, fat, and eggs. In his diet, red and fat meats dominated over lean meats. He was eating vegetables in insignificant amounts. His diet had a ketogenic ratio (fat:protein + carbohydrate) of at least 2:1. No oil of plant origin or artificial sweeteners were allowed.
He also took 5,000 IU of vitamin D3 and excluded all milk and dairy from his diet [two important dietary strategies that we will address later].
The best part is that it didn’t take six months for the combination of the paleolithic ketogenic diet with vitamin D supplementation to produce results. In fact, the tapering of insulin was done promptly. Researchers stated that “following the first paleolithic-ketogenic meal glucose level was only 86 mg/dL thus there was no need for external insulin.”
However, there is some bad news. These case studies only reflect what happened to one young girl and one adolescent male on a ketogenic type diet. This means that these results may not apply to other type 1 diabetics. We need some evidence from larger studies as well. Luckily, there are two.
In one study consisting of twenty-two patients with type 1 diabetes, carbohydrate restriction was put to the test. While they were on a diet that limited them to 70-90 g carbs per day, participants had significantly less hypoglycemic (low blood sugar) episodes, lower A1C levels, and required less insulin after three months of carbohydrate restriction.
A similar result was found in another study on 48 people who had type 1 diabetes for 12 years or longer. They were simply educated on how to reduce carbohydrate consumption and lower their insulin dosages. Twenty-three of the participants were adherent to the “diet” and experienced a significant decrease in A1C after three months and four years.
Even without a strict ketogenic diet protocol, carbohydrate restriction helped type 1 diabetics. This suggests that carbohydrate restriction is highly effective in improving type 1 diabetes management.
But what about reversing type 1 diabetes? It is highly unlikely that this is possible. According to the current evidence, the most that a diet can do for a patient with type 1 diabetes is halt disease progression and reduce their insulin needs. In cases where the patient is still able to produce some insulin, it is possible for them to be taken off of insulin medication completely with the help of the right diet and healthcare professional.
Two Important Considerations for The Ketogenic Diet & Type 1 Diabetes
If we look closely at the paleolithic-ketogenic diet that the 19-year-old male implemented, we can find some clues to his outstanding success. The researchers made two important adjustments to the classic ketogenic diet that helped the subject halt disease progression, restore some insulin production, and manage type 1 diabetes without any medication.
1. Vitamin D Supplementation
Vitamin D helps modulate the innate and adaptive immune responses. This means that it can help prevent and reverse the autoimmune issues that commonly cause type 1 diabetes.
In fact, it is important for everyone to supplement with vitamin d3 or daily sun exposure due to the potential consequences of Vitamin D deficiency.
For example, infants and young children who are vitamin D deficient may be imprinted for the rest of their lives with increased risks of type 1 diabetes, multiple sclerosis, rheumatoid arthritis, and many common cancers.
The simplest way to obtain vitamin D is from moderate exposure to sunlight. For more specific guidelines, many experts suggest supplementing daily with 4,000 IU vitamin D3 without sun exposure or 2,000 IU plus 12–15 minutes of midday sun.
2. The Elimination of Immune System Provoking Foods From The Diet
Wheat and cow’s milk have been reported to cause strong immune system reactions in type 1 diabetic patients. Something that occurs less often in nondiabetics.
Consumption of cow’s milk has also repeatedly been shown to increase the risk of type 1 diabetes. Some scientists suggest that the milk protein may promote autoimmune processes and give rise to the condition. In fact, two case reports from the literature found that the classic ketogenic diet, which contains a significant amount of dairy, lead to the development of type 1 diabetes in a couple of children with epilepsy.
This doesn’t indicate that dairy can cause type 1 diabetes, but it most definitely can be an accelerator of the disease. Wheat sensitivities may also accelerate the condition by causing gut issues that make type 1 diabetes harder to manage.
The paleolithic-ketogenic diet limits wheat, dairy, and carbohydrate consumption making it the most promising type 1 diabetes diet we know of so far. This is because it not only normalizes glucose levels but may also halt autoimmune processes mediated by milk protein and wheat gluten as well.
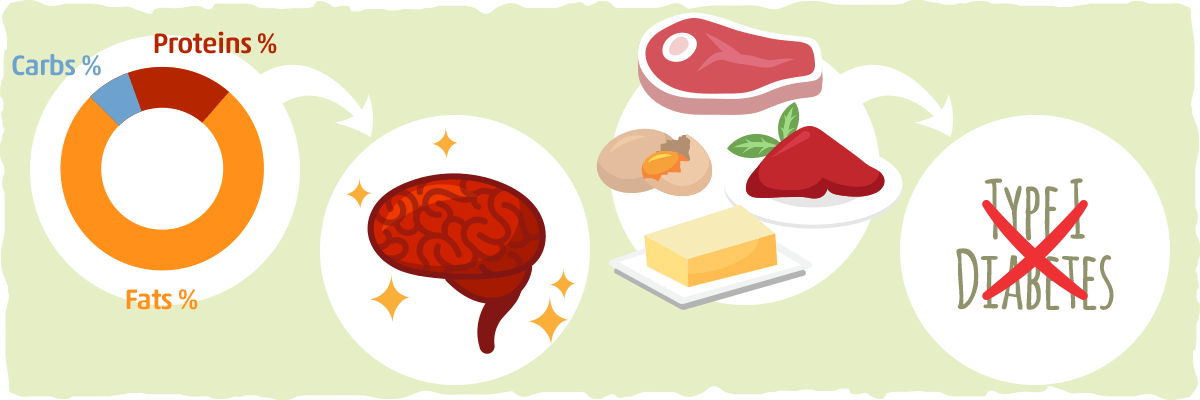
The Takeaway — What is The Best Type 1 Diabetes Diet?
Type 1 diabetes and the keto diet may be the best match for some diabetes patients. In fact, the current data suggest that both low carb and ketogenic diets are highly effective for improving type 1 diabetes management.
Overall, the roadmap for an ideal type 1 diabetes diet may look something like this:
- Follow a ketogenic diet (less than 30 grams of carbohydrates per day)
- Restrict the consumption of dairy and wheat products to see if insulin production improves
- Supplement with vitamin D3
Although these three dietary rules seem simple enough to follow, diabetes patients are likely to experience dramatic changes throughout the body. This will include lower blood sugar levels, decreases in A1C, changes in insulin sensitivity, weight loss, and nutritional ketosis (i.e., healthy increases in ketone level, not diabetic ketoacidosis).
As a result, diabetes medication dosages — insulin dose in particular — will likely need adjustment to accommodate the changes in carb intake and blood glucose levels.
This is why it is vital to work together with your doctor while implementing any major dietary change, such as a ketogenic or low carb diet, to ensure effectiveness and safety.
Is The Keto Diet Safe For Type 1 Diabetes?
Though the keto diet is safe and effective for weight loss and type 2 diabetes management, those with type 1 diabetes will require closer monitoring and diabetes medication adjustments to ensure safety. If carbohydrate intake and insulin dose are not changed simultaneously on a low carb or keto diet, the risk of hypoglycemia increases significantly.
Once this is addressed, it is important to ensure that the keto or low carb diet is well-formulated with plenty of healthy fats, low-carb vegetables, and enough calories (so that you don’t lose weight unexpectedly).
How to Know if Your Treatment Plan is Working
One way to see how well your plan is working is by tracking your A1C levels and aiming for specific blood sugar levels throughout the day.
Your target A1C goal may vary depending on your age and various other factors, but the American Diabetes Association generally recommends that A1C levels should be below 7 percent. A1C testing is one of the best indicators of how well your diabetes treatment plan is working. An elevated A1C level may signal the need for a change in your insulin regimen, meal plan or both. This measurement should be taken at least every three months.
In addition to the A1C test, the doctor will also take blood and urine samples periodically to check your blood sugar levels, cholesterol levels, thyroid function, liver function and kidney function.
The goal is to keep your daytime blood sugar levels before meals between 80 and 130 mg/dL (4.44 to 7.2 mmol/L) and your after-meal numbers no higher than 180 mg/dL (10 mmol/L) two hours after eating.
As long as you are not plagued by unexpected stress, blood sugar and A1C levels will decline while you are on the ketogenic diet. However, even when both A1C and blood sugar levels are normal, it is still important to monitor blood sugar levels and administer the appropriate amount of insulin.
When insulin is not used in the proper amounts at the right times, an unhealthy amount of ketones can build up in the blood and cause diabetic ketoacidosis. (For more on diabetic ketoacidosis, click here.)
Conversely, when insulin is available, ketone production is kept from getting out of control. This allows a healthy amount of ketones to be released into the blood, providing an alternative fuel source and many other benefits. (For more on ketones and their benefits, click here .)
Putting It All Together Into a Type 1 Diabetes Diet and Lifestyle
Having a normal life with type 1 diabetes is possible. In fact, most people with type 1 diabetes can manage the condition in such a way that they can reduce insulin requirements and improve their health and well-being.
Here is a quick recap of the diet and lifestyle:
- Determine an effective treatment plan with your doctor.
- Implement a ketogenic diet that limits dairy and wheat consumption.
- Check blood sugar levels frequently throughout the day (at least 8-10 times).
- Supplement with vitamin D3 by getting sun exposure and taking a supplement every day.
- Exercise daily, but make sure you monitor your blood sugar and check for hypoglycemia symptoms.
- Get your A1C levels tested every three months to determine the effectiveness of your treatment plan.
For more on the ketogenic diet and how to get started, check out our beginner’s guide.
Sources:
- Type 1 Diabetes — Mayo Clinic
- Innate immunity and intestinal microbiota in the development of Type 1 diabetes — NCBI
- Type 1 diabetes: new perspectives on disease pathogenesis and treatment — Science Direct
- Vitamin D: importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis — The American Journal of Clinical Nutrition
- Type 1 diabetes and epilepsy: Efficacy and safety of the ketogenic diet — Wiley Online Library
- Type 1 Diabetes Mellitus in Pediatrics — Pediatrics in Review
- Type 1 diabetes mellitus successfully managed with the paleolithic ketogenic diet — Edorium Journals
- The “Perfect Storm” for Type 1 Diabetes — NCBI
- A low carbohydrate diet in type 1 diabetes: clinical experience–a brief report. — NCBI
- Benefits of Sunlight: A Bright Spot for Human Health — NCBI
- Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study — BioMed Central