How our cells respond to hormones dictates, to a large extent, how healthy we are.
For example, when our cells aren’t sensitive to the effects of insulin (one of the main anabolic and energy-storage hormones in the body), we have a higher chance of developing metabolic diseases such as diabetes, obesity, and heart disease.
In contrast, insulin sensitive cells are able to efficiently and effectively respond to insulin in a way that allows us to carry out many of the vital mechanisms needed to maintain health.
Altogether, this phenomenon is called insulin sensitivity, and it plays a significant role in fat loss, hormone balance, metabolic function, and disease prevention.
Fortunately, you won’t be stuck at a specific level of insulin sensitivity for the rest of your life. In fact, there are several strategies you can use to increase your receptivity to insulin — but before we can implement them, we must take a closer look at the intriguing phenomenon of insulin sensitivity.
What is Insulin? The Lifesaving Effects of a Highly Misunderstood Hormone
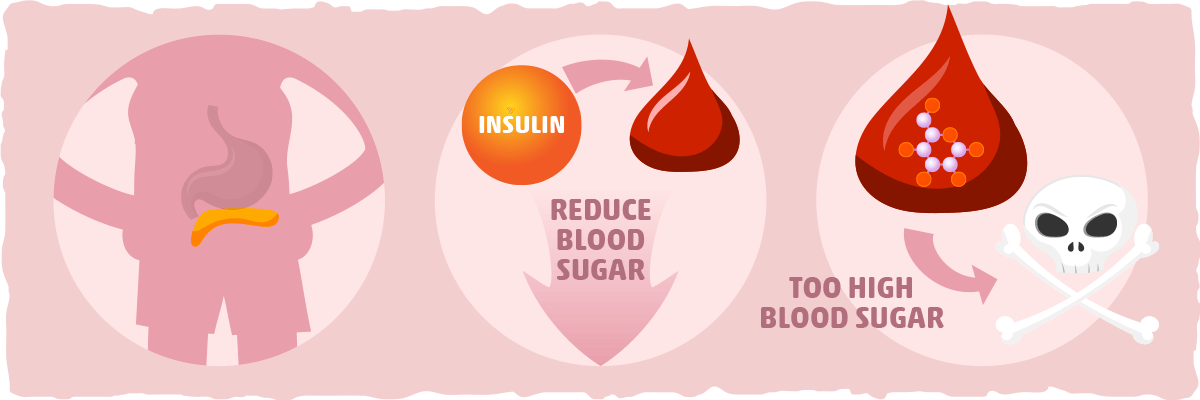
Insulin is a protein based hormone secreted by the pancreas in response to increases in blood sugar. Insulin’s primary role is to regulate the nutrients you absorb from food, primarily carbohydrates.
When you eat and digest carbs, it increases how much sugar is in your bloodstream. This is detected by the cells in your pancreas which will then secrete insulin into the blood.
Once the insulin is traveling in your bloodstream, it starts to facilitate the uptake of sugar into the cells that need energy.
The purpose of this action is to reduce the amount of sugar in your blood and trigger the cells to use it and/or store it. This is essential for our health because abnormally high amounts of sugar in the blood can cause harm throughout the body. In some cases, having high blood sugar levels can even cause major health issues and become fatal if not managed properly.
Dispelling Some Common Myths about Insulin
In the keto community, insulin is typically known as our “fat storage hormone.” Although there is some truth to this (because insulin tends to stimulate sugar burning and shut down fat burning and ketone production), the hypotheses that arose from this understanding are not supported by the evidence.
For example, one of the most popular explanations for the growing obesity epidemic is that our carb-heavy diets keep our insulin levels so high that it prevents us from burning stored fat. This is known as the “Carbohydrate-Insulin Hypothesis,” and it’s touted as the main reason for why low carb diets, like the ketogenic diet, are so effective at boosting fat loss.
Basically, all you have to do is cut out the carbs, and you will lower insulin levels, trigger fat burning, and lose fat, right?
This hypothesis is accurate in some aspects, but seeing insulin and fat loss in this way neglects the bigger picture. When we consider the totality of the biochemistry and physiology of digestion and energy metabolism, insulin is simply one piece of information that feeds into what the body decides to do.
Put in another way: insulin provides our cells with info regarding glucose availability and energy status, and our cells will integrate that information with all the other information they have about their own energy status, needs, and abilities to come up with the appropriate actions.
The ultimate result is that cells burn energy when they need fuel and stop burning energy when they don’t — insulin is just one of the hormones involved in the decision making process of the cells. This means that your energy intake (i.e., calorie consumption) is the ultimate arbiter of whether you gain or lose weight. Insulin is but one of the many factors that determine what you do with the calories you consume, and insulin sensitivity is the key to unlocking insulin’s full potential.
What is Insulin Sensitivity?
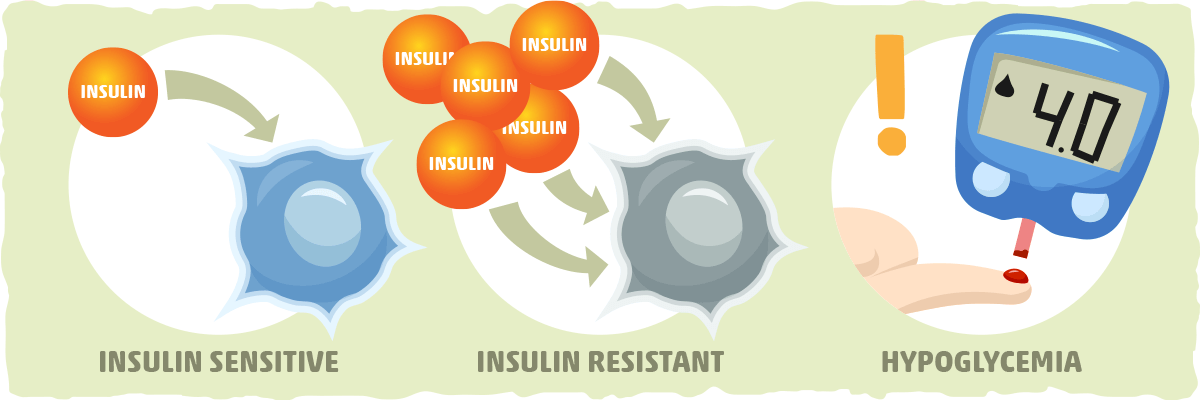
Insulin sensitivity is the term that we use to describe how the cells in our body respond to insulin. The more insulin sensitive your cells are, the more responsive they will be to insulin, and vice versa.
To measure this phenomenon objectively, we need to figure out how much insulin your body needs to produce to deposit a certain amount of glucose (sugar). You are considered insulin sensitive if your body only needs to secrete a small amount of insulin to deposit glucose into the cells, and you are considered insulin resistant when you need a higher than normal dose of insulin for the cells to respond.
For most people, having good insulin sensitivity is essential for having good overall health. There are some rare cases, however, when being too insulin sensitive can be harmful.
For example, people who have type 1 diabetes may increase their risk of hypoglycemia (blood sugar below 4 mmol/L) if they are too insulin sensitive. In general, people who are on insulin or other medications that help manage blood sugar levels must be cautious of the changes in their blood sugar that occur when they exercise and make other adjustments to their lifestyles that increase insulin sensitivity.
The Three Different Types of Insulin Sensitivity
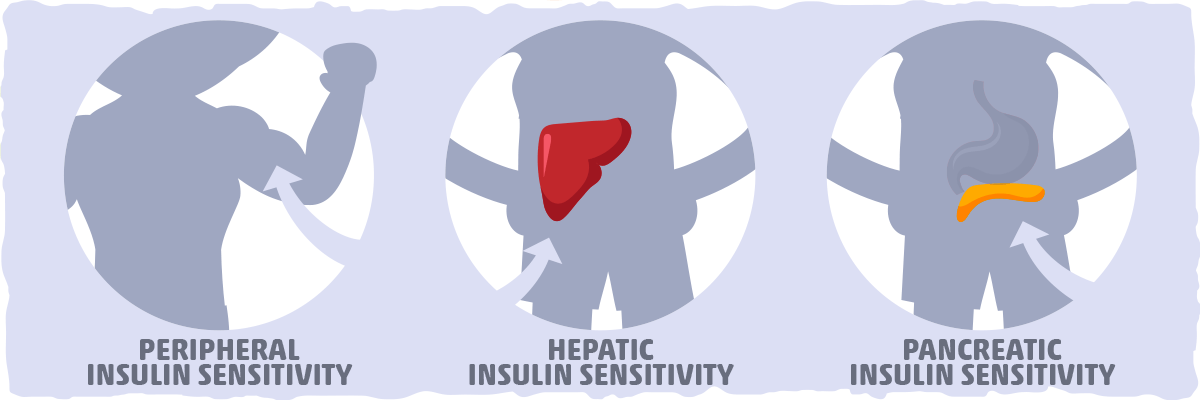
There are three different kinds of insulin sensitivity:
- Peripheral insulin sensitivity. This is how accepting your muscle and fat cells are of glucose either when stimulated by insulin or by themselves. The most common form of insulin resistance is found in the muscle and fat cells. This is typically caused by inactivity (lack of muscle use) and overeating (excess energy availability).
- Hepatic insulin sensitivity. This influences the process of gluconeogenesis (the production of blood sugar from non-sugar substrates). Insulin plays a crucial role in regulating this process, and its effects can be blunted by the presence of liver inflammation.
- Pancreatic insulin sensitivity. This relates to the actual operation of the cells that produce insulin (i.e., the beta cells). If the beta cells aren’t functioning properly, insulin resistance can develop. This typically happens as a result of conditions like type I diabetes (insulin insufficiency) and Cystic Fibrosis (where the function in physically hindered).
The Main Attraction: Peripheral Insulin Sensitivity and Weight Loss
Insulin sensitivity has turned into a widespread phenomenon in the weight loss industry because of the strong correlation between peripheral insulin sensitivity and body fat percentage.
The research literature suggests that the more insulin sensitive you are, the more carbohydrates your body can convert into energy without storing it as fat. Thus, if you want to lose weight, it is probably best to make sure you are optimizing your insulin sensitivity.
What Determines Your Insulin Sensitivity?
Both modifiable and non-modifiable factors determine the degree to which you are insulin sensitive or insulin resistant.
Non-modifiable factors are factors that cannot be changed. Some examples of non-modifiable factors that decrease insulin sensitivity are:
- Increasing age. Although it is possible to prevent the decline in insulin sensitivity with certain lifestyle changes, research has found increasing age to be associated with increased insulin resistance.
- Genetics. Specific genes can determine how sensitive certain cells are to insulin. For one example of what I mean by this, check out our article on polycystic ovary syndrome — a condition that is intimately linked with cells that were left vulnerable to insulin resistance by specific genes.
- A family history of type 2 diabetes. The combination of genetic and environmental factors that come with your family history can leave you with a higher risk for decreased insulin sensitivity.
- Ethnic background. If you are of African-American, Asian-American, Latino/Hispanic-American, Native American or Pacific Islander descent, you have a greater likelihood of developing insulin resistance.
In contrast, the modifiable factors — what you can actually do to increase your insulin sensitivity — are
- losing weight
- reducing stress levels
- eating fewer carbohydrates
- exercising
- getting adequate sleep
- taking specific supplements and/or drugs that decrease insulin resistance
- maintaining a calorie deficit
- fasting/intermittent fasting
- and many more that we will take a closer look at later in this article
By neglecting to use these modifiable risk factors to your advantage, you will steadily reduce your insulin sensitivity and set the stage for insulin resistance and the conditions that come with it.
The Opposite End of the Spectrum: Weak Insulin Sensitivity, Insulin Resistance, and Diabetes

Low insulin sensitivity can be detrimental to your health, especially when your sensitivity is so low that you develop insulin resistance.
When we become insulin resistant, the pancreas starts creating more insulin to help decrease blood sugar levels. This leads to high insulin levels, otherwise known as “hyperinsulinemia.”
Hyperinsulinemia is linked to blood vessel damage, high blood pressure, osteoporosis, and heart disease. Over time, having chronically high levels of insulin and blood sugar will cause health to deteriorate.
If left untreated, insulin resistance can cause your cells to become even more insulin resistant via a positive feedback loop.
In other words, the cells in your body will lose their insulin sensitivity, and both your blood sugar levels and insulin go up. Eventually, the insulin-producing cells (beta cells) will start to lose their ability to function, blood sugar levels will continue to increase, and you will develop type 2 diabetes.
If this condition is left untreated, it can become lethal (which is exemplified by the fact that type 2 diabetes is one of the top 10 causes of death worldwide).
Fortunately, this vicious cycle of insulin resistance can be prevented — and its severity significantly reduced — when we address the lifestyle factors that drive insulin resistance.
The Big Picture — Insulin Sensitivity and Insulin Resistance
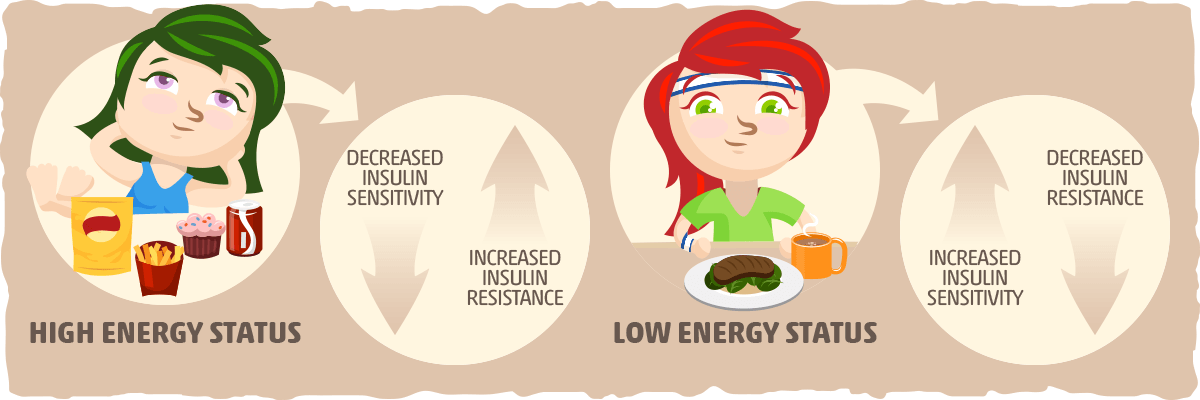
The physiology of insulin sensitivity is so complex that we aren’t even close to explaining it all. However, it is possible to distill our learnings into one simple concept that will help you understand what causes insulin resistance and insulin sensitivity for most people:
- Increased energy status will cause your cells to become more insulin resistant and less insulin sensitive over time.
- Decreased energy status will cause your cells to become less insulin resistant and more insulin sensitive over time.
By energy status, I mean the current state of your cells. Are they being bathed in energy molecules without any demand to use it up? This is “high energy status”, and it occurs when we are inactive and overeat.
But what if your cells are in need of more energy to keep up with your body’s demands? Then this indicates that you are in “low energy status”, and your cells will increase their sensitivity to insulin so that they don’t miss out on the opportunity to get more fuel.
To further illustrate the big picture of insulin sensitivity, here is a graph from an article published in Comprehensive Physiology:
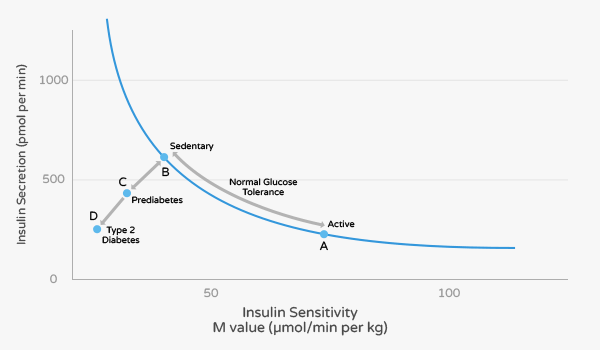
This graph depicts the relationships between insulin secretion and insulin sensitivity. Insulin secretion rises as insulin sensitivity falls when an individual goes from a state of exercise training/being physically active (point A) to inactivity/sedentary (point B). In contrast, insulin secretion decreases as insulin sensitivity increases when a person goes from inactivity/sedentary (point B) to physically active (point A). This is what commonly occurs in healthy individuals.
However, when insulin secretion fails to compensate for a fall in insulin sensitivity, the person will progress to prediabetes (Point C). If no changes are made at this point, the disease will progress from point C to Point D (type 2 diabetes). The only way to prevent this from happening is by improving your insulin sensitivity.
What Causes Insulin Resistance?
Although the exact cause of insulin resistance and type 2 diabetes is not yet fully understood, researchers have found the most robust evidence for the following two factors:
- Overeating — When we eat more food than our body needs, our cells will naturally become more insulin resistant. This will also cause weight gain and elevated blood glucose levels. If this dietary pattern continues for the long term, our likelihood of developing insulin resistance and metabolic syndrome increases substantially.
- Visceral fat — This is the type of fat that accumulates around our organs, creating what is often called a “potbelly” or “beer gut.” Visceral fat has been found to secrete inflammatory hormones and free fatty acids that drive insulin resistance.
Other potential causes of insulin resistance include:
- Excess fructose intake — Diets high in added sugars that contain fructose are strongly associated with insulin resistance, particularly in the liver.
- Chronic inflammation — Increased oxidative stress and inflammation throughout the body can impair insulin signaling and reduce insulin sensitivity.
- Lack of physical activity — Inactivity drives insulin resistance while moving more than usual will increase insulin sensitivity.
- An imbalanced gut microbiome — Evidence suggests that a disruption in the balance of beneficial gut bacteria can increase inflammation and insulin resistance.
Various genetic and social factors can contribute to our likelihood of developing insulin resistance as well. However, this doesn’t mean some of us are destined to get type 2 diabetes.
Even if you weren’t born with the best genetics for insulin sensitivity, you can still vastly decrease your risk of insulin resistance by implementing the lifestyle tips below.
10 Ways to Improve Insulin Sensitivity
Luckily, insulin sensitivity isn’t a fixed mechanism in the body. It can be drastically improved with simple lifestyle modifications.
Here are ten proven ways to help enhance your insulin sensitivity:

1. Follow the Ketogenic Diet
Carbohydrates stimulate the most insulin release of all the macronutrients so, theoretically, a low-carb diet should decrease insulin levels and improve insulin sensitivity to some degree.
The current research seems to back up this speculation. In one study, for example, ten obese subjects with type 2 diabetes (i.e., they all had high levels of insulin resistance) consumed their regular diet for one week, followed by a low carb high fat ketogenic diet for two weeks.
After the two weeks of keto dieting, there was a 30% decrease in overall caloric intake and a drastic 75% increase in insulin sensitivity. Similar findings are being echoed throughout the research, which we took a closer look at in our article on the ketogenic diet and insulin resistance.
However, carbohydrate restriction is not the only reason why keto dieting can help with insulin resistance. The keto diet provides with insulin sensitivity boost that we get from fat loss as well.
2. Lose Fat
Studies have shown that having high amounts of fat, especially around your midsection, can produce harmful chemicals and hormones responsible for decreased insulin sensitivity and increased inflammation.
Simply by losing excess fat, insulin sensitivity and metabolic function will improve significantly. More specifically, one study found that a weight loss of 5 percent is all obese patients need to experience some of the positive effects of fat loss on insulin sensitivity.
For more specific recommendations, check out our article about how to lose weight on keto.
3. Implement Fasting and/or Intermittent Fasting
We learned earlier that decreased energy status typically leads to increased insulin sensitivity. Although losing weight is one way to achieve a lower energy status, sprinkling in some fasting and/or intermittent fasting throughout your diet plan can help as well.
In fact, one pilot study found that intermittent fasting for 2 weeks (with a 18-20 hour feeding window) helped to improve blood sugar levels with a trend toward improved insulin sensitivity in type 2 diabetics.
The research on dietary interventions for type 2 diabetes also suggests that calorie restriction is one of the major factors that can help manage and potentially reverse the disease. One way to achieve this, which was confirmed by the pilot study on intermittent fasting, is by restricting your feeding window, so you eat fewer calories throughout the day.
By eating fewer calories, you decrease your energy status, which improves overall insulin sensitivity.
However, there is one caveat to fasting and intermittent fasting for people who have diabetes. Since both forms of fasting can cause significant changes in blood sugar levels, it is best to consult your doctor before adding these strategies to your lifestyle.
4. Add Aerobic and Anaerobic Exercise to Your Weekly Schedule
One of the quickest ways to improve insulin sensitivity is by exercising. Exercise has such an impact on our energy stores that many of the cells throughout our body must make themselves more sensitive to insulin to ensure that they will get the energy they need.
Fortunately, both aerobic and anaerobic exercise will reduce your insulin resistance in a variety of ways, so the type of exercise you do is entirely up to you.
Aerobic exercise involves any form of physical activity that you requires you to exercise for a prolonged period of time without rest breaks. This includes jogging, swimming, or anything where you’re moving your body at a steady state for 30 minutes or longer.
Aerobic activity has the ability to increase insulin sensitivity for up to 72 hours after the exercise session. Anaerobic exercise, like lifting weights, sprinting, and intense rowing/cycling, can also drastically improve your insulin sensitivity.
In contrast, being sedentary or purposely restricting your activity levels, can decrease your body’s insulin sensitivity significantly, increasing your chances of becoming insulin resistant. This is part of the reason why most of us need to move more.
Overall, it is best to aim for five hours of exercise per week. Research suggests that this is the sweet spot for vastly improving your insulin sensitivity.
To get the best results, I recommend doing a combination of aerobic and anaerobic exercise throughout the week. Anaerobic exercise will help you build more muscle and burn through glycogen stores, which keeps your insulin sensitivity high, while aerobic exercise will burn off sugar and trigger fat burning, so that your cells never have a chance to increase their insulin resistance.
5. Get Adequate Sleep Every Night
Having a set sleep schedule that allows you to get at least 7 hours of sleep every night is essential for proper hormonal function.
When you lack sleep, your body’s hunger hormone, ghrelin, begins to fluctuate, and your cortisol levels elevate. In other words, losing sleep will cause you to feel hungrier than usual while simultaneously increasing your stress levels and insulin resistance (thanks to cortisol).
Altogether, these hormonal changes will typically cause you to eat more and struggle to regulate glucose effectively when you do have those extra calories. The best way to counteract this is by going to sleep at the same time every night and waking up at around the same time every day after getting at least 7 hours of sleep.
6. Reduce Your Stress Levels
Not only is cortisol released to help you wake up in the morning, but it is also secreted when your body goes through any physical, mental or environmental stress.
When cortisol is circulating through the blood, it stimulates various mechanisms in your body that increase your blood sugar levels, providing you with the energy you need to handle the stressful situation. One way that cortisol does this is by increasing insulin resistance.
Once the body has taken care of the stress-inducing situation, cortisol will be broken down and insulin sensitivity restored. This response to stress is healthy and normal — in the short term.
However, it is not uncommon for people in modern society to be stressed for the majority of the day. With every stressor comes more cortisol, decreased insulin sensitivity, and more stress. The only way to stop this cycle is by giving your body a chance to relax and recover from your daily stressors.
Here are some helpful ways to reduce your stress levels:
- Meditate
- Take a short nap
- Do yoga, tai chi, and/or qi gong
- Quit smoking
- Exercise regularly
- Maintain a good sleep schedule
- Use adaptogenic herbs like Rhodiola and Ashwagandha
- Supplement with vitamins and minerals that you may be deficient in (magnesium and vitamins C, E, B, and D, in particular, can help with stress)
7. Consume More Soluble Fiber
Of the two types of fiber, insoluble and soluble, soluble fiber is most notable when it comes to insulin sensitivity. This is because soluble fibers slow down the movement of food through the small intestines, which helps reduce the amount of sugar that enters your blood, decrease appetite, and lower cholesterol levels.
Due to how it is digested, many studies have discovered that soluble fiber has a positive effect on improving insulin sensitivity. This means that incorporating foods high in soluble fiber such as low carb vegetables, keto bread, or supplementing with Psyllium Husk capsules can increase your sensitivity to insulin as well.
8. Add More Low Carb Fruits, Vegetables, Herbs, and Spices to Your Diet
Many studies have found that a diet rich in plant compounds from fruits and vegetables is linked to higher insulin sensitivity. The healthiest plants tend to be low-carb fruits and vegetables like wild berries, leafy greens, and cruciferous vegetables. For more specific recommendations on what to eat, feel free to check out our low-carb fruit guide and our low-carb vegetable guide.
Herbs and spices have also shown promising results for boosting insulin sensitivity. Here are some of the most effective:
- Turmeric. This powerful herb contains an active component called curcumin, which has potent antioxidant and anti-inflammatory properties. It can indirectly increase insulin sensitivity by reducing free fatty acids and sugar in the blood.
- Ginger. This popular spice is linked to increased insulin sensitivity as well. Studies have found that its active component, gingerol, makes muscle cells more receptive to sugar.
- Garlic. In animal studies, garlic has been shown to improve insulin secretion. It also has antioxidant properties that may directly increase insulin sensitivity.
- Cinnamon. This savory spice is most well-known for its ability to reduce blood sugar and increase insulin sensitivity. For example, one meta-analysis found that consuming 1/2–3 teaspoons (1–6 grams) of cinnamon daily significantly reduced both short and long-term blood sugar levels. Other studies have discovered that cinnamon has various properties that can help promote efficient glucose absorption.
9. Drink Green Tea
Green tea is an excellent beverage for your overall health.
It’s also an excellent choice for people who are struggling to manage their blood sugar levels. Several studies have found that drinking green tea can increase insulin sensitivity and reduce blood sugar.
The beneficial effects of green tea could be due to its powerful antioxidant epigallocatechin gallate (EGCG), which many studies have found to increase insulin sensitivity on its own.
To add green tea to your diet (and get the benefits of burning fat for fuel), try our Iced Ketoproof Green Tea. On the other hand, if you are trying to avoid caffeine consumption, supplement with decaffeinated green tea extract instead.
10. Experiment with Supplements that Boost Insulin Sensitivity
There are many supplements that can help with insulin sensitivity, but let’s stick with the ones that are backed by research:
- Resveratrol. This is a polyphenolic compound that can be found in red wine and is known for its antioxidant benefits. Regarding insulin sensitivity directly, high-quality evidence indicates that resveratrol can boost glucose uptake as well.
- Alpha Lipoic Acid. Alpha Lipoic Acid (ALA) is an organosulfur compound that is essential for aerobic metabolism. Many studies have reported that supplementation with this compound helps to reduce insulin resistance in subjects with type 2 diabetes.
- Berberine. This is a plant alkaloid that has been shown to lower blood glucose in many cases. Some researchers have even found berberine to be as effective as the anti-diabetic medication metformin.
- Chromium. Some evidence indicates that this essential trace element has the ability to enhance the effects of insulin and decrease blood glucose levels.
- Magnesium. This essential mineral is so crucial for the effectiveness of insulin that magnesium deficiency can worsen insulin sensitivity.
As with taking any supplement, make sure to consult with your doctor — especially if you are taking medications.
How to Know If You Are Insulin Sensitive
The quickest and safest way to find out if you are insulin sensitive is to get a test done by your doctor. The most reliable test is called HOMA-IR, which makes an accurate guess regarding your body’s insulin resistance by tracking your blood sugar and insulin levels.
You can also measure your blood sugar fluctuations directly with an oral glucose tolerance test. This test consists of multiple blood tests and the ingestion of a glucose solution as a way to see how your body handles an increase in blood sugar levels.
However, despite how helpful these tests are, both of them are inconvenient and unnecessary for most people. A more accessible way to track insulin sensitivity is by seeing how your blood work and other health indicators change as you make the appropriate dietary and lifestyle adjustments.
For example, if your blood sugar levels, blood lipids, and blood pressure reach healthier levels, then you are most likely improving your insulin sensitivity and optimizing your health. Furthermore, if you are losing weight and inches off your waist, then you are almost certainly making your cells more sensitive and less resistant to insulin.
Putting It All Together — Everything You Need to Know about Insulin Sensitivity
Insulin plays a crucial role in regulating your blood sugar levels (and it performs many other functions throughout the body as well). However, just because insulin is released and interacts with our cells doesn’t mean our cells will respond to it the same way every time.
In fact, depending on various factors, your cells may be more insulin sensitive (i.e., more responsive to the effects of insulin) or more insulin resistant (i.e., not as responsive to insulin). By adopting a lifestyle that fosters more insulin sensitivity, you can decrease your likelihood of having too much insulin resistance and the issues that are associated with it (i.e., obesity, type 2 diabetes, heart disease, and various other health conditions.)
To increase your sensitivity to insulin, try implementing some of these strategies:
- Follow the keto diet
- Lose fat
- Exercise
- Implement fasting or intermittent fasting protocols
- Get at least 7 hours of sleep a night following the same sleep cycle
- Add stress-relieving activities to your daily life
- Consume more soluble fiber
- Eat more low-carb fruits, low-carb vegetables, herbs, and spices
- Drink green tea or take green tea extract
- Take supplements that have been proven to help with insulin sensitivity
You will get the biggest bang for your buck out of following a diet that helps you maintain a calorie deficit (e.g., the keto diet), losing fat, and exercising regularly.
To make losing fat and being in a calorie deficit as easy as possible, try adding strategies 4 through 8 to your lifestyle. Not only will each one help improve insulin sensitivity, but they will help you lose more weight and improve your overall health as well. Supplements and green tea should only be used as a way to boost the results you are already getting from the other lifestyle changes you decide to make.
After you’ve made some of these adjustments, you can either get some tests done to see how you’ve improved or use proxy measures, like your weight, blood work, and waist circumference, to track improvement indirectly. Unless you have diabetes and need to monitor your insulin resistance for medical reasons, I recommend using the proxy measures. For most people, improved blood work numbers, waist circumference reduction, and weight loss are reliable indicators of increased insulin sensitivity and overall health improvement.
To help you find out exactly what to eat and drink to optimize for insulin sensitivity and a calorie deficit to get the keto diet results you want, check out the resources below:
- How to Lower Blood Sugar Naturally
- Hundreds of Keto Recipes: Breakfast, Lunch, Dinner, Snacks, Side Items, and Condiments
- The impact of a keto diet and diabetes
- The Best Low Carb Vegetables for Keto
- Best Low-Carb Fruits (and Which to Avoid)
Sources
- The role of adipose tissue dysfunction in the pathogenesis of obesity-related insulin resistance. — NCBI
- Metabolic Syndrome and Insulin Resistance: Underlying Causes and Modification by Exercise Training — NCBI
- Insulin sensitivity in the intact organism. — NCBI
- 14 Natural Ways to Improve Your Insulin Sensitivity — Healthline
- How do I increase insulin sensitivity? — Examine
- Changes in beta cell function occur in prediabetes and early disease in the Leprdb mouse model of diabetes — NCBI
- Understand Your Risk for Diabetes — American Heart Association
- The top 10 causes of death — World Health Organization
- Understanding Insulin Sensitivity and Diabetes — National Institutes of Health
- Insulin Resistance and Hyperinsulinemia — American Diabetes Association
- Insulin resistance and associated compensatory responses in african-american and Hispanic children. — NCBI
- Racial/Ethnic Differences in Insulin Resistance and Beta Cell Function: Relationship to Racial Disparities in Type 2 Diabetes among African Americans versus Caucasians. — NCBI
- Effects of long-term calorie restriction and endurance exercise on glucose tolerance, insulin action, and adipokine production. — NCBI
- Ethnic Differences in the Relationship Between Insulin Sensitivity and Insulin Response — American Diabetes Association
- Effect of alpha-lipoic acid on blood glucose, insulin resistance and glutathione peroxidase of type 2 diabetic patients. — NCBI
- Oral magnesium supplementation improves insulin sensitivity and metabolic control in type 2 diabetic subjects: a randomized double-blind controlled trial. — NCBI
- Chromium — WebMD
- Effects of resveratrol on glucose control and insulin sensitivity in subjects with type 2 diabetes: systematic review and meta-analysis — NCBI
- The impact of soluble dietary fibre on gastric emptying, postprandial blood glucose and insulin in patients with type 2 diabetes. — NCBI
- Mechanisms of Glucocorticoid-Induced Insulin Resistance — NCBI
- Effects of intensity and volume on insulin sensitivity during acute bouts of resistance training. — NCBI
- Aerobic training improves insulin sensitivity 72-120 h after the last exercise session in younger but not in older women. — NCBI
- Effects of short-term, medium-term and long-term resistance exercise training on cardiometabolic health outcomes in adults: systematic review with meta-analysis. — NCBI
- Exercise and insulin sensitivity: a review. — NCBI
- In obese patients, 5 percent weight loss has significant health benefits — ScienceDaily
- Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. — NCBI
- Effects of intermittent fasting on health markers in those with type 2 diabetes: A pilot study — NCBI
- Insulin Resistance Isn’t All About Carbs and Insulin — Chris Masterjohn, PhD
- The Biochemistry of Why Insulin Doesn’t Make You Fat — Chris Masterjohn, PhD
